
A cascade of knowledge
Training the trainers with Jackie Matthews
Long-standing medical volunteer Jackie Matthews, has recently returned from the first Sub-Saharan Africa ‘Patient Management and Community Health Initiatives’ workshop, in the heart of Antananarivo, Madagascar. Jackie has been sharing her knowledge and expertise with local teams including patient and programme coordinators, and representatives from all nine Sub-Saharan African countries where Operation Smile works: Ghana, Ethiopia, Democratic Republic of Congo, Rwanda, Kenya, Malawi, Mozambique and Madagascar.
With a nursing background of 23 years, Jackie works at Guy’s and St Thomas’, as a clinical nurse specialist in cleft. This experience enabled her to take on the role of clinical lead during the workshop and she covered key areas of training including identifying cleft conditions, early intervention, feeding babies with cleft, and psychosocial care. She tells us more:
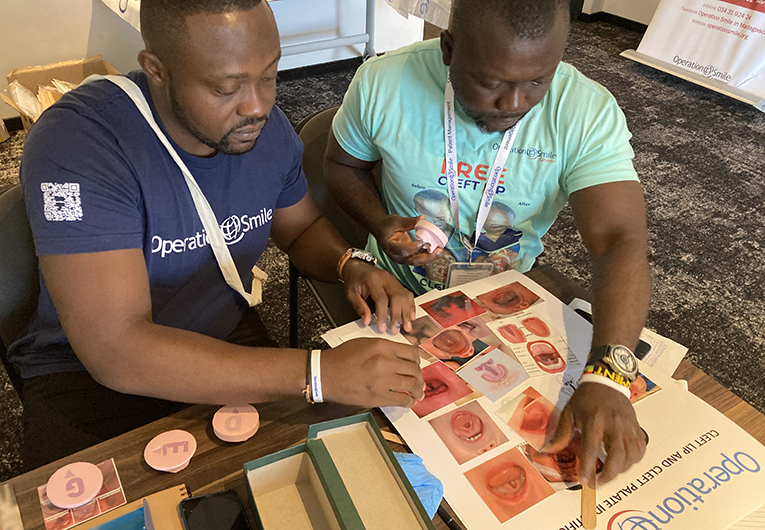
“Our focus was on leading with empathy and compassion, and we did some amazing work. They were such an engaged group, and very willing and happy to be there. We talked about how to engage with families, how it might feel to be a parent of a baby with a cleft, and how to react and engage with parents and carers. Then we looked at understanding cleft conditions, what’s a normal palate, what’s a palate with cleft, what’s a cleft lip and all the different definitions. In addition to photographs, we used 3D models of the different cleft conditions to give them a really good understanding of each type of cleft and what they look and feel like. This is about training the trainers, so they will use these models in the field to increase understanding i.e. ‘This is what a cleft palate looks like in the mouth – this is what you might see inside a baby’s mouth.’”
In addition to group sessions and presentations, there were practical activities as well to ensure delegates got a thorough understanding of the challenges faced by children with cleft conditions and their families. Jackie explains, “I gave them all a little tumbler of water with a drinking straw. And I’d cut the drinking straw so that they were trying to drink through the straw, but with a cut straw. So, they’re sucking like mad, but not able to get much liquid up at all – which demonstrates how much energy a child with a cleft palate expends trying to feed.”
The delegates used mannequins and dolls to practice feeding babies with cleft, and Jackie showed them how to correctly position a child during feeding, using feeding cups and special bottles, as well as highlighting common feeding problems and how to tackle them. “These techniques help babies to be well nourished so they can get to our programmes, get surgery, and live a full life. So it’s hugely important!” She told us.

Because of problems feeding, malnutrition is a major problem for children with cleft conditions, so the delegates also learned about Operation Smile nutrition programmes from Nutrition Lead and Director of Comprehensive Care at Operation Smile, Charlotte Steppling.
This type of hands-on training is fundamental in helping local teams identify cleft conditions early so that less children have to grow up with the burden of an untreated cleft. “A key focus of the week was on education and early intervention, which I’ve been talking about for such a long time.” Jackie explains. “We need to get to these patients, and make sure that they can have safe surgery, but more than that, so we can identify them and get them help as early as we can. To do this we need to spread the word and educate people. While in Madagascar, we worked on the production of some animated films to help raise awareness – these will be dubbed with the local language so that everyone can understand, which is another way of spreading the word.”
The delegates also spent an afternoon at the patient village, where patients stay when they arrive at a surgical programme. Jackie tells us, “When we arrived, the patients and their families were all there singing and dancing – it’s really moving when you see them all together. We also showed the delegates around so that they could see what the patients and families do while they are at the village, and the different stages of care. Then we looked at the ‘compassion booth’ a Madagascar team initiative – which is such a good idea – where patients who don’t get selected for surgery can go for additional support and advice, such as referral to the nutrition programme or for medical treatment.”
We asked Jackie what the next steps would be for the patient coordinators who attended the training, and she was in no doubt about the positive impact of the week’s sessions. She said:
“Throughout the week, we built strong communication and active listening skills, grew mutual trust and a collaborative approach to the team dynamic. The workshop enabled a spirit of teaching and learning, sharing and exchanging of knowledge and importantly, displayed the essence of Operation Smile – a commitment to excellence, care, integrity and compassion, and growing love for the next generation.

“I think the only way is up, as far as they’re concerned, the patient coordinators left with a bag full of training aids and materials to take with them. They’ve got posters and tangible tools to teach with. They’re fired up with enthusiasm, inspired by each other’s stories and experiences too. The feedback has been entirely positive, and the training week has enabled the group to move forward with new strategies and ideas – I’m sure they will hit the ground running and do great things because they’ve got so much enthusiasm and compassion! It’s going to make a world of difference in the field, reaching more families!”
Jackie hopes the training can be used as a model for future workshops and says: “I hope we can take this training elsewhere because it’s been so successful and worth its weight in gold. A lot of work has gone into it, but it’s such a valuable thing. If you can really train the trainer, then it’s a cascade. You get that knowledge, and it just seeps through and spreads the word!”